Interlaminar technique
In interlaminar surgery, the access to the spinal canal is done via the posterior interlaminar window. The dilator is guided directly to the flavum ligament with a dilator without prior puncture. After placing the working sleeve over the dilator, the operation is performed through the high-resolution diskoscope under continuous irrigation. The functionality of the components of the access system and the instruments are precisely coordinated. It even allows to pass through the ligamentum flavum and the nerve root with minimal traumatization.
With special manual instruments and a variety of high-speed burrs available, bone parts of spinal stenoses can be resected under a full-endoscopic view.

VERTEBRIS stenosis
- High resolution 4K endoscopes with shorter working length and increased irrigation rate for full-endoscopic interlaminar approach stenosis surgery.
- Endoscope adapter to control the distance between endoscope and working sleeve for more ergonomic operation.
- Optimized ratio of large working channel (5.6 mm) to outside diameter (10.5 mm) for least invasive access trauma and highly effective operation.
- Fluid management optimized by engineered dimensioning of inflow and outflow preventing neural compression by high pressures of the irrigation fluid.
- Working Sleeves with atraumatic distal design to protect neural structures.
- Stable grasping forceps and punches with overload protection and shorter working length for interlaminar approach.
- Large diameter (5.5 mm) bone punches and Kerrison punches for rapid and precise manual bone removal.
- Endoscopic high-speed drill system with a variety of large diameter reusable and disposable burrs for mechanical bone resection of laminae and facet.
- TipControl instruments for 4 MHz radiofrequency coagulation and ablation, and hollow tip RF probes for large scale tissue coagulation and ablation.
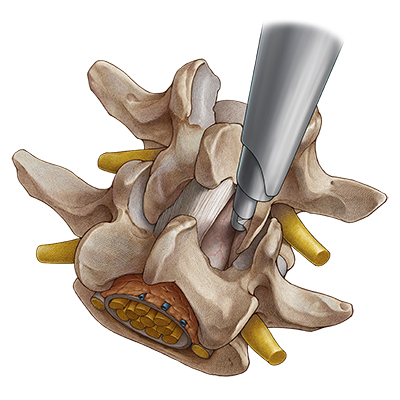
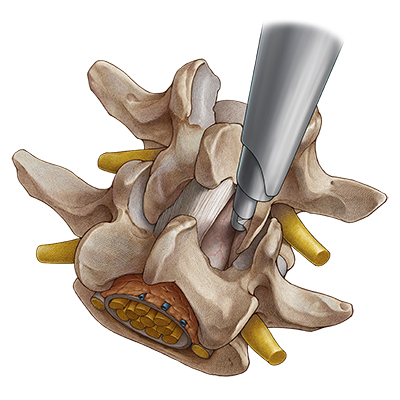
Ipsilateral decompression on one side
After the access has been created, the bony structures are exposed. It may be helpful to start decompression at the caudal end of the descending facet. Depending on the pathology, decompression is then commenced with resection of parts of the medial descending facet, the cranial and caudal lamina, and the ligamentum flavum. The extent of decompression generally continues cranially at least until the tip of the ascending facet and caudally to half of the pedicle. The medial portions of the ascending facet and the ligamentum flavum are then resected until sufficient decompression of the neural structures can be clearly seen – cranially, caudally and laterally. In the case of a central stenosis, the ligamentum flavum generally needs to be resected medially to the midline. Finally, it may be necessary to remove protruding annulus parts and osteophytes in the ventral epidural space.

Contralateral decompression in over-the-top technique
If bilateral symptoms occur with a central stenosis, a unilateral approach is carried out with “over-the-top” access using the undercutting technique to the opposite side. For this purpose, bone in the ventral area of the spinous process is resected until the contralateral side can be accessed dorsally up to the dura of the spinal cord. If possible, the ligamentum flavum is initially left in place to protect the dura and bony decompression is again carried out by laminotomy and partial facetectomy. The ligamentum flavum is then completely resected. Finally, the contralateral recess needs to be extended. The decompression is completed when the dura and the spinal nerves have been clearly decompressed.
An extended and uninterrupted excessive retraction of the neural structures with the working sleeve in a medial direction must be avoided particularly in cranial areas, or only carried out intermittently, in order to avoid the risk of neurological damage. Experience indicates that as with all new techniques there is generally an enhanced risk of problems occurring during the learning curve.




Reviews
There are no reviews yet.